More than a decade ago, the Institute for Better Health at Trillium Health Partners was founded with a bold vision to lead the coalition for better health through scientific expertise, innovative thinking, and strong partnerships.
Our 2024-25 Annual Report captures how we bring our vision to life and highlights our amazing team, partners, patients, families, and community members who inspire us to do things differently, champion change, and shape a healthier tomorrow. In the stories that follow, we share on-the-ground examples of how our work is truly helping create a new kind of health care for a healthier community.
Health systems are under immense pressure. An aging population, growing health complexities, widening inequities, and persistent capacity challenges demand immediate and lasting change. At the Institute for Better Health, we meet these challenges head-on, by moving knowledge into action and co-designing solutions with our team, patients, caregivers, and community partners to create better health.
As we look to the future, we remain committed to pushing the boundaries of what’s possible, ensuring that the work we do today sets the foundation for a healthier tomorrow.
Our accomplishments over this past year would not be possible without the continued support of the team at the Institute for Better Health and our hospital. Most importantly, we thank our patients, families, and community members for your partnership in creating a healthier, more inclusive tomorrow. Together, we are curing health care for everyone.
AI for Better Health: Accelerating for Human-Centred Impact
As one of the busiest hospitals in the country, serving one of the largest and most diverse communities in the world, Trillium Health Partners is uniquely positioned to shape the future of health care innovation in Canada. From AI-powered discharge planning to community-driven diabetes prediction and prevention, we are already seeing what’s possible when we match our people’s expertise with the right tools and technologies.
Launched in 2024, our AI for Better Health program represents a fundamental leap forward in creating a new kind of health care for a healthier community. By equipping our teams with powerful, practical AI tools, we can better predict and prevent illness, improve patient and team experience, and ease pressure on our health system. This initiative will help us advance a new era of health care that is safer, smarter, and more connected — both at the point of care and across the community.
Co-designing AI solutions


Last year, the Institute for Better Health hosted the fifth Hazel McCallion Lecture in Shaping Healthier Communities, spotlighting AI for Better Health through real-world examples from across the hospital and community. The event demonstrated how we’re using AI to enhance human capabilities and foster equitable, person-centred care.
The Lecture reinforced that successful implementation and adoption of AI solutions starts with a collaborative approach to identify the real-world challenges faced by health care and community providers. Human-centred AI solutions are “centered around the patient,” says Aderemi (‘Remi) Ejiwunmi, Vice President, the future Shah Family Hospital for Women and Children at Trillium Health Partners. “Ensuring we [point-of-care teams] are using tools to allow us to make care more accessible to patients, see patients as a whole person, and help make our job easier as [health care] providers in a challenging environment.”
A case in point is a partnership between long-term care residence Wellbrook Place, RxFood, PointClickCare, DIGITAL and the Institute for Better Health on a project to use clinically proven AI nutritional assessment technology to assess their residents’ food intake. Traditionally, health care staff use notetaking to estimate the percentage of food consumed. With one photo, the AI tool analyzes a resident’s food tray and estimates the amount of each food item remaining, how much was consumed, and the nutritional value. This innovation delivers a detailed and accurate snapshot of a resident’s nutritional health, enabling clinicians to make more informed patient care decisions, streamline food ordering, and reduce food waste.
Building Diverse and Inclusive Data Sets


For AI tools to be effective, they require diverse data sets that reflect the populations they serve. Without diverse data, AI solutions risk developing biased algorithms that exacerbate existing biases in health care and fail to address the needs of all patients.
In the Peel Region, Dr. Laura Rosella, Chief Scientist and Stephen Family Research Chair in Community Health at the Institute for Better Health, is co-leading an AI for Diabetes Prediction and Prevention Solutions Network to partner with the community to responsibly deploy machine learning models to inform diabetes prevention and management. This involves building a comprehensive diabetes dashboard for the Peel Region, one of Canada’s most demographically diverse communities, which will account for the complex demographic and social factors that are essential to consider in addressing diabetes in populations.
The Network brings together local community members, health care providers, and policy makers who discuss and provide feedback on the dashboard. “AI tools for use in public health and health care are ultimately intended to impact peoples’ health and well-being,” says Dr. Rosella. “If we want to ensure that goal will be accomplished in a positive way without any harm, we need to work directly with community members to shape the way AI tools are designed and deployed.” Through the Network, community members can bring up valuable questions and considerations, including the importance of transparency and diversity in who is developing AI models, as well as the need for a better understanding of AI at the community level.
Partnering for Real-World Impact
Last year, Trillium Health Partners announced a multi-year partnership with Signal 1, a Canadian health AI company, to further develop its internal AI capabilities and accelerate the safe, ethical, and responsible adoption of AI tools.
The partnership is the first time that Signal 1’s full technology suite, including its industry-leading AI platform, will be deployed across a hospital network in Canada. A key pillar of the partnership is developing the right culture, skills, and structures to promote the safe acceleration of AI within Trillium Health Partners. This includes the development of an overarching AI governance approach for the organization informed by evidence and co-designed with experts.
The partnership involves a comprehensive suite of AI-based applications to improve quality of care, patient flow, and operational effectiveness. One example, but not the only use case, is an expanded Discharge Solution. This tool, which has been deployed in Credit Valley Hospital’s Medicine unit since 2023, helps care teams identify patients who may be ready for discharge by supporting them with timely, data-informed insights. By flagging potential discharges early, the tool helps staff coordinate next steps, reduce unnecessary delays, and free up beds for incoming patients.
The new solution (Pilot 2) includes an updated model being retrained on a significantly larger and more diverse data set to provide greater accuracy and updated workflows that have been informed by clinical and other end-user feedback and experiences from the first pilot deployment.
The Institute for Better Health’s Data Platform is an advanced cloud-based data repository that allows for advanced analytics and played a crucial role in training and evaluating this discharge readiness prediction model. This year, a multidisciplinary team of data scientists and architects at the Institute for Better Health facilitated its retraining to enhance accuracy. The Data Platform has continued to be a cornerstone for research, innovation, and operational excellence, supporting multiple high-impact projects that are shaping the future of health care.
The future of AI in health care depends on our ability to centre people – patients, providers, and communities – very step of the journey. By viewing AI as a tool built with diverse data sets to amplify human capabilities, the Institute for Better Health and Trillium Health Partners are unlocking its full potential to create a healthier community.
Partnering with Patients, Families and Communities to Advance Population Health
Here are some of the ways the Institute for Better Health connected with our community this year, working alongside people and organizations to drive meaningful change and improve health and well-being in the community.
Digital Bridge: Supporting Seamless Transitions from Hospital to Home
The Digital Bridge to Home project is improving what happens after patients leave the hospital. Co-led by the Institute for Better Health and Sinai Health, this initiative co-designs digital health tools with patients, caregivers, and clinicians to enhance communication and care coordination during hospital-to-home transitions.

The project integrates patient-identified needs, such as real-time updates on discharge planning and care team communication, into technology solutions that support a smoother recovery process. “Patients and caregivers told us they need better visibility into their care plans,” explains Dr. Terence Tang, Clinician Scientist at the Institute for Better Health and one of the project’s principal investigators (alongside investigators from Sinai Health’s Science of Care Institute and Lunenfeld-Tanenbaum Research Institute). “By embedding these insights into digital tools, we’re making the transition home safer and less stressful.”
Engaging Diverse Voices: Creating Better Cancer Diagnosis Pathways
In partnership with Ontario Health (Cancer Care Ontario), the Institute for Better Health’s Moonshot Collaborative for Translational Health Equity is leading a pilot project to centre the voices of structurally marginalized communities in redesigning how cancer is diagnosed.
Led by Dr. Ibukun Abejirinde, Scientist at the Institute for Better Health, alongside Nuzha Hafleen, Isabelle Choon and Asli Hersi, the project has established three separate engagement tables with Black, Francophone, and Newcomer patients and care partners across Ontario.
“This project brings forward the voices and lived experiences of people from diverse backgrounds to help shape a cancer diagnosis process that is more responsive, equitable, and inclusive for everyone in Ontario,” says Richa Tewari, Newcomer Peer Project Advisor.
“The engagement tables have been transformational beyond our expectations. Each has evolved into a community of advocacy and care, offering participants a sense of belonging and a safe space to be heard,” says the Engaging Diverse Voices project team. “Their collective motivation to inform an equitable and harm-free cancer journey has become a catalyst for personal healing and systems transformation. Importantly, the team at Ontario Health (Cancer Care Ontario) has been listening and is committed to using these insights to inform responsive diagnostic pathways.”
This equity-oriented initiative offers a replicable and actionable model for meaningfully engaging structurally marginalized groups in health service re-design – ensuring that the perspectives of those most affected by inequities are not only heard but are at the forefront of shaping change.
Recognizing and Supporting Caregivers Through Research and Co-Design
Caregivers – whether family members, friends, or neighbours – play a critical yet often invisible role in the health care system. As the number of caregivers in Canada continues to grow, with approximately one in four people over the age of 15 being a caregiver, so does the need to better identify, support, and integrate them into health and social care teams.

A new four-year study led by Dr. Kerry Kuluski, Scientist and Dr. Mathias Gysler, Research Chair in Patient and Family Centred Care at the Institute for Better Health, is responding to this challenge. Guided by a caregiver advisory panel from the Peel Region and in partnership with the Canadian Centre for Caregiving Excellence, the study will generate evidence and practical solutions to ensure caregivers receive the recognition and support they deserve.
From the outset, caregivers will be active partners in shaping the research, contributing to the development of new tools, resources, and best practices for caregiver integration. “This research matters because it will gather local and global evidence of how caregivers are supported and integrated in health care,” says Bhavini Patel, one of the study’s caregiver advisors. “Having been a caregiver in the Region of Peel, I see how bringing this research to life by creating and implementing programs and support services will be essential for the growing number of caregivers in this diverse community.”
This initiative has the potential to transform how caregivers are recognized, supported, and integrated into care, with local, national, and global impact. By shining a light on and working alongside these often-unacknowledged individuals, we take an important step toward a more inclusive and compassionate health care system.
Partnering with the Community to Address Youth Diabetes in Peel
The Peel Family Diabetes Awareness Program is part of the Family and Child Health Initiative, co-led by Dr. Ian Zenlea, Clinician Scientist at the Institute for Better Health and Division Head and Medical Director of Children’s Health at Trillium Health Partners; and Dr. Dianne Fierheller, Scientist and Community Engagement Lead at the Institute for Better Health. The program, supported by the Trillium Health Partners Foundation and Sun Life, is partnering with South Asian and Black, African, and Caribbean communities to help understand and overcome current social, environmental, and systemic barriers and lack of family-centred services to address rising type 2 diabetes rates. This project is a partnership between Trillium Health Partners, Indus Community Services, Roots Community Services, Punjabi Community Health Services, Dixie Bloor Neighbourhood Centre, Wellfort Community Health Services, and LAMP Community Health Centre.


This initiative will advance diabetes education and prevention at the grassroots level to address the individual, family, and community challenges of type 2 diabetes. Trained health coaches from two organizations – Punjabi Community Health Services and Wellfort Community Health Services – are working with and supporting adolescents and caregivers at risk for type 2 diabetes to provide education and awareness to better manage their health, help prevent type 2 diabetes, and provide wraparound community support.
Using a community and health equity lens, this program will provide valuable insights into the factors that affect the implementation and outcomes of these efforts and contribute to identifying the most effective pathways to prevent type 2 diabetes in these diverse communities.
These patient-and community-centred initiatives exemplify the Institute for Better Health’s commitment to co-designing health solutions that reflect the realities of patients, families, and communities. They reinforce a simple truth: health care works best when it is shaped by those who experience it firsthand.
Championing Black Excellence at the Institute for Better Health: Paving The Way for Future Health Care Leaders
At the Institute for Better Health, we are dedicated to mentoring the next generation of health scientists and researchers to shape the future of health care and help build equitable, healthy communities. On May 1, 2024, the Nurturing Black Excellence program was launched to nurture, elevate, reward, and amplify research and innovation excellence in Black-identifying health researchers.
“Systemic barriers for Black professionals are rooted in historical injustices that perpetuate systems of oppression and exclusion,” says Dr. Ibukun Abejirinde, Scientist at the Institute for Better Health who curates the program. “These experiences can discourage young Black professionals and impact career advancement. The Nurturing Black Excellence program is aligned with our commitment at the Institute for Better Health to dismantle anti-Black racism and become an institution that drives positive change.”


The program began with a pilot for Black-identifying graduate students (masters, doctoral, medical) conducting short-term placements at the Institute for Better Health under the supervision of an Institute for Better Health Scientist or Research Chair. The experience includes hands-on research projects with a principal investigator, regular engagement with a senior executive leader, thematic conversations, group activities, and peer mentorship. “The level of ownership and collective commitment of Institute for Better Health team members to contribute to the program has been remarkable,” says Dr. Abejirinde. “They have invested their time, resources, and networks.”
Since the program’s inception, five trainees have been enrolled, and their time at the Institute for Better Health has been defined by hands-on research, deep collaboration, and personal growth. “I’ve learned so much and have met so many people,” says Tiya Samuel, a Master of Public Health student in the Black Health stream at the Dalla Lana School of Public Health, University of Toronto. “I appreciate the connections I’ve built at the Institute for Better Health.” Samuel contributed to a project on equity and Learning Health System data collection under the supervision of Dr. Azza Eissa, Clinician Scientist at the Institute for Better Health. Her reflections on her time at the Institute for Better Health underscore the importance of being embedded in a thriving professional community through thoughtful engagement and mentorship.
Asli Nur, a Master of Public Health student, was drawn to the Insititute for Better Health’s focus on race-based data collection, a critical area that influences health equity. Under the supervision of Health Equity Research Lead, Dr. Nakia Lee-Foon, she explored the potential benefits and risks of gathering demographic data in hospital settings and presented her insights to key health system leaders. She later returned to the Institute for Better Health as a Nurturing Black Excellence Program Coordinator, working alongside Dr. Abejirinde to document lessons learned and support the program’s continued growth.
Ijeoma Itanyi, a Ph.D. candidate specializing in Artificial Intelligence and Data Science in Public Health at the University of Toronto, also saw an opportunity at the Institute for Better Health to bridge cutting-edge research with real-world impact. As part of her placement, Itanyi supported Chief Scientist Dr. Laura Rosella’s AI for Diabetes Prediction and Prevention project, co-facilitated a community engagement strategy co-design session, collaborated on a manuscript, and contributed to grant writing efforts all while navigating a personalized Nurturing Black Excellence learning journey focused on leadership, networking, and career growth.
Through programs like Nurturing Black Excellence, the Institute for Better Health offers learners the opportunity to have transformational experiences that will springboard them to success in their future careers. We are grateful for the trainees that have brought their professional development, creativity, insights, and expertise to the Institute for Better Health, and are optimistic about the future of health care in their hands.
Building a Learning Health System, Together
What if health care could learn, adapt, and improve in real time, with teams that work across traditional boundaries? That’s the vision behind a Learning Health System – an approach where patients, caregivers, community members, researchers, health care leaders, and the care teams come together to continuously learn together and improve health care. Every interaction with the health system is an opportunity to learn; where knowledge, feedback, and data are quickly applied to shape better, more person-centred care.
In a Learning Health System, explaining this concept in a way that resonates with patients and families is as important as its implementation. That’s why researchers at the Institute for Better Health collaborated with a diverse group of patients, caregivers, and community members from across Canada to co-create an easy-to-understand comic that brings the Learning Health System to life. Supported by the Ontario Strategy for Patient-Oriented Research Support Unit, the team explored how to make the Learning Health System concept accessible, relatable, and actionable through a series of virtual workshops – because a true learning system starts with people who understand and see themselves in it.
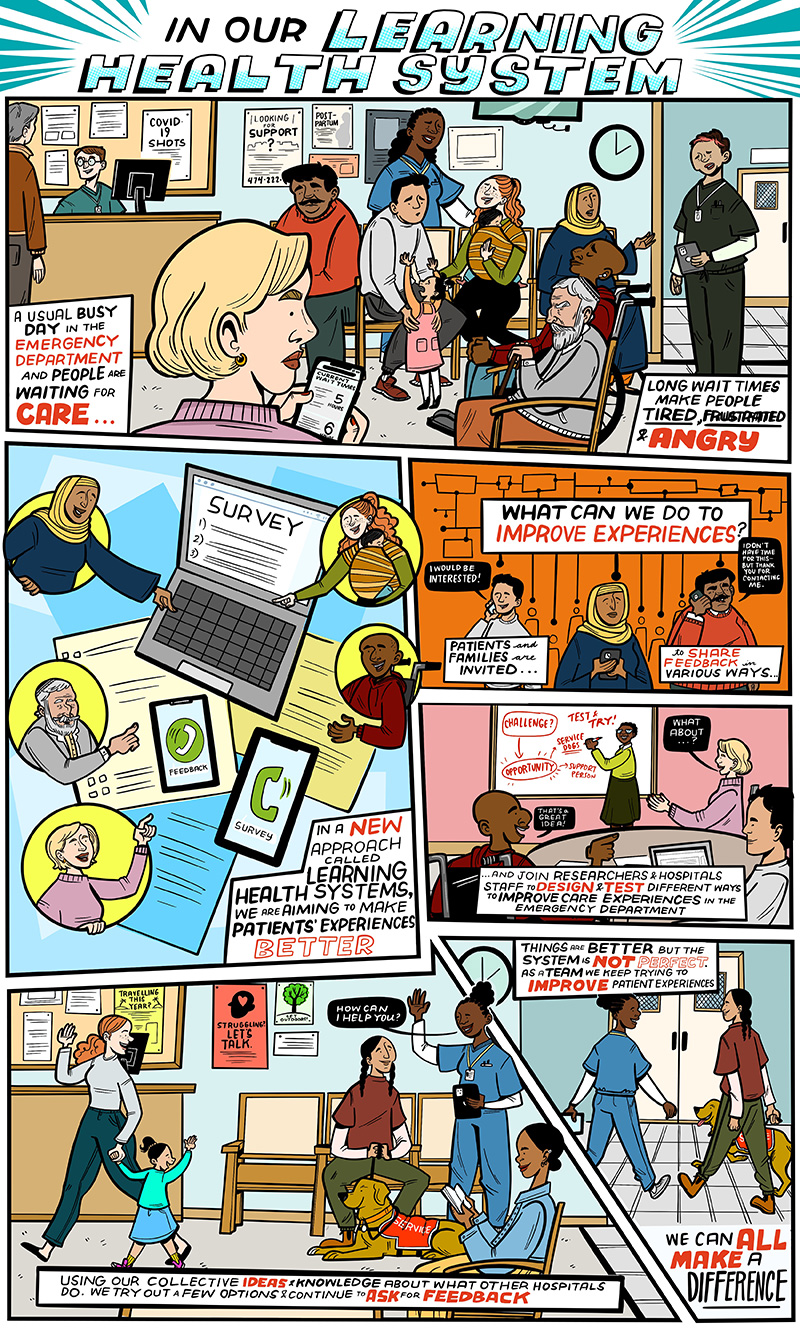
From co-designing educational tools to projects that accelerate on-the-ground impact, the following highlights showcase the ways the Institute for Better Health is driving the Learning Health System into action.
Learning Health System in Action: Cataract Care
Access to cataract care can be life changing. Dr. Matthew Schlenker, Glaucoma, Cataract and Advanced Anterior Segment Surgeon and Investigator at the Institute for Better Health, and his team are applying a Learning Health System approach to better understand and redesign the journey from vision loss to diagnosis and surgery. By embedding data and patient- and community-informed perspectives into every phase of the work, the team is helping to build a more responsive, inclusive, and equitable system for cataract care.
The team conducted interviews with patients, optometrists, family physicians, and ophthalmologists to explore how decisions are made, what barriers exist, and how these experiences affect people’s lives. Through semi-structured interviews, they heard from patient participants: “I thought it was normal to lose vision;” “I didn’t know there was something I could do to fix it;” “It wasn’t until I had a car accident that they checked my eyes and noticed something was wrong.” Interview findings were paired with clinical insights and population-based analysis of access to eye care in Canada to reveal inconsistent referral criteria, missed opportunities for early intervention, and the significant impact of vision loss on quality of life.
Complementing this work is a recently published study on risk communication in cataract surgery, led by Dr. Schlenker’s team. The results highlighted the importance of how information is communicated, reinforcing the need for patient-centred education and reflection on how risk is perceived by patients. This work directly supports the development of patient-centred tools to improve decision-making and informed consent in cataract care.
The project is now laying the foundation for a new, patient and provider informed model of cataract care, including developing tools to help providers assess surgery appropriateness, building dashboards to track wait times, and designing educational resources to improve awareness. By integrating research, data, and lived experience, this work is a clear example of a Learning Health System in action to shape a smarter, more equitable future for eye care.
Supporting Teams to Learn Together

The Institute for Better Health Accelerator Grant competition engages multidisciplinary teams of scientists, researchers, learners, and Trillium Health Partners operational leaders to advance innovative and impactful research that helps respond to key challenges needed to improve the health of the Peel population. The projects address questions that are of interest to more than one team or department to help encourage learning across siloes.
Through the generous support of the Trillium Health Partners Foundation, Accelerator Grant funding was awarded across four research projects. “This funding program was tailored to create impact by supporting emerging and early-stage research ideas that will provide the insights needed for larger co-design efforts, evaluations, and trials while also building Learning Health System capacity at Trillium Health Partners,” says Dr. Laura Desveaux, Scientific Director and Learning Health System Lead, the Institute for Better Health. “These project teams bring together leaders and professional staff from Trillium Health Partners, community partners, patients, and scientists and are a testament to the growth in both our Learning Health System capabilities and collaborative relationships in the pursuit of improving population health and shaping a healthier tomorrow.”
Case in point is a project led in collaboration with Trillium Health Partners’ Women’s and Children’s Program. The project aims to begin developing a women and children learning health care community that bridges the hospital with the community and broader health system. It will explore, co-design, and pilot the collection of sociodemographic data for individuals accessing the Women’s and Children’s Program at Trillium Health Partners and community services across the Peel Region, laying the groundwork for more equitable, person-centred women’s and children’s care across the system.
Advancing Learning Health System Leadership: Launch of the Learning Health Systems Academic Certificate
In 2024, the Institute for Better Health partnered with the Dalla Lana School of Public Health at the University of Toronto to launch the first phase of a Learning Health Systems Academic Certificate Program. This new professional development opportunity designed specifically for health system leaders and operators is the first of its kind in Canada.
This certificate program equips health care leaders with the knowledge, tools, and practical experience to embed a Learning Health System approach into their operational environments, directly aligning with Trillium Health Partners’ academic mandate to continuously teach, discover, innovate, and learn to inform health care transformation, creating a Learning Health System. “In today’s health care landscape, ambiguity and rapid change are the norm,” says Dr. Laura Desveaux, Scientific Director and Learning Health Systems Program Lead at the Institute for Better Health. “The Learning Health Systems Certificate Program is designed to support leaders to move beyond adaptation to actively driving meaningful improvements.”
Phase 1 of the program was piloted in fall 2024 with a small group of leaders from across Trillium Health Partners whose work already reflects Learning Health System principles. The immersive, six-module format focused on knowledge-building and skills development. Participants explored real-world cases, reflected on current challenges, and applied new tools designed to improve quality, equity, and population health outcomes.
“The Learning Health System course empowers health care leaders to drive meaningful, equity-centred transformation across the entire system,” says Mary Ackie, Manager, Clinical and Patient Services, Mental Health Program at Trillium Health Partners. “It offers practical tools to align research and health care delivery, fostering continuous improvement in outcomes, experiences, and sustainability. Most importantly, it calls for a new way of thinking about change management, one that embraces learning, adaptability, and equity at its core.”
This first phase also laid the foundation for program evaluation and future scaling. With input from learners and faculty alike, Phase 2 will launch in 2025 as a fully accredited academic offering for a broader audience across Ontario and Canada. “By fostering a culture of shared learning and evidence-based improvement, we not only strengthen leadership but lay the foundation for a system that better responds to the needs of the people it serves,” says Dr. Desveaux.
The certificate builds on the Institute for Better Health’s leadership in Learning Health System innovation – further deepening its collaboration with point-of-care teams, academic partners, and community leaders to shape a stronger, more responsive health system.
Fostering and Celebrating Innovation at the Point of Care
Last year marked a major milestone in the evolution of Trillium Health Partners’ mission to create a new kind of health care for a healthier community as the Institute for Better Health announced the launch of the Core Innovation Program.
Innovation lies at the heart of our ability to shape a healthier future, and the Core Innovation Program is dedicated to supporting high-impact innovation from point-of-care teams that is aligned with Trillium Health Partners’ goals of improving quality, access, and sustainability. It also addresses the critical issues facing health care at Trillium Health Partners and in the community.
The program is supported by the Trillium Health Partners Foundation through a transformational gift from the Orlando Corporation. It will be designed with input from our point-of-care teams to support staff in tackling some of the biggest challenges we face today, ensuring that their ideas have the platform and support they need to thrive.
The Core Innovation Program builds a supportive environment where bold ideas can be transformed into practical solutions. It also facilitates the development and spread of innovative solutions generated by people at the point of care. We are passionate about nurturing a culture and community of innovation at Trillium Health Partners. Through innovation, we can shape a healthier future for our patients, families, and the community.
One of the program’s key activities is the Innovation Awards, which happens annually during Patient Safety, Quality, and Innovation Week. Last year, 29 innovations were submitted, all of which are changing how the team at Trillium Health Partners works, cares for patients, and creates better health. Here are a few highlights.

Service Innovation
The Innovation “Emergency Department Point-of-care Ultrasound Archiving Initiative”
The Team Dr. Alice Chan, Dr. Andrea Unger, Dr. Kyle Pasternac, Avneet Bhatia, Poonam Patel, Alexander Cheong, Linda Szymanski, Jessica Belerique, Andy Zapata, Alex Pankov, Jack Wong, and Florian Roche
The Impact “We successfully implemented a new point-of-care ultrasound archiving system in the emergency department whereby images are uploaded to the hospital's picture archiving and communication system and integrated into the electronic health record. This is a first-of-its-kind solution in North America, which significantly improves the quality of care, medical education, and patient and family experience.” – Dr. Alice Chan, Physician, Emergency Medicine & Critical Care

Access Innovation
The Innovation “Wellbrook Long-Term Care Home Geriatric Medicine Clinic”
The Team Dr. Jason Kerr, Dr. Abhishek Narayan, Joanna Ellis, Jennifer D’Alessio, Dr. John Gong, Dr. Mini Joshipura, Dr. Amina Jabbar, Dr. Vesna Page, Karen Hunter, Dawn Foley, Florence Paat, Domenico De Bellis, Dr. Errol Sequeira, Ruben Rodriguez, Mira Memelli, Colleen Hunter, Caitlin Reidy, Ather Rizvi, Rajwinder Dhanju, Felix Gayongorsa, Fiorinta Flammia, Deslyn Willock, and Allan Frost
The Impact “By bringing Trillium Health Partners’ geriatric specialists into long-term care homes, we can improve access to care for residents. At Trillium Health Partners, we’re proud to lead the way in providing innovative and collaborative care, but we know our work here isn’t done. We look forward to scaling this model, as well as sharing lessons learned with external partners in the hope of expanding system wide.” – Dr. Jason Kerr, Division Head, Seniors Services

Sustainable Innovation
The Innovation “Optimizing the Education and Care of Heart Failure Patients”
The Team Victor Lam, Melissa Murray, Dr. Hanna Lee, Dr. Tahseen Rahman, Nadzeya Karatigin, Julia Carter, Marie Maccena, Gracy Mathew, Shoko Jairam, Sonia Perez, Yeony Choi, Nancy Rodrigues, Dana Jackson, Hailey Knott, Khrisette Linay, Rosanna Lee, Alesia Letta, and Amna Al-Khayat
The Impact “A new virtual heart failure education class is helping patients better manage their condition while reducing strain on the health care system. Since its launch, cardiologists and nurse practitioners have observed a downward trend in hospitalizations; and patient confidence in managing diet and medication has improved from 60 to 75 per cent.” – Victor Lam, Clinical Pharmacist, and Melissa Murray, Registered Dietitian

Trailblazer Innovation
The Innovation “Introduction of Flexible Endoscopic Evaluation of Swallowing”
The Team Bon-Hi Moon, Dr. Janet Chung, Dayani Gomes, Andrea Tersigni, Mia Misic, Anna Boron, Lisa Sacco, and Dayna Jablecki
The Impact “In December 2023, Trillium Health Partners introduced a new bedside assessment tool called Flexible Endoscopic Evaluation of Swallowing, which provides a real-time, direct view of a patient’s swallowing function using a small endoscope. To make this possible, Speech-Language Pathologists partnered with the Otolaryngology team to receive specialized training and delegation, allowing them to bring this innovative service directly to inpatients. By increasing access to objective swallowing assessments at the bedside, this collaboration is improving patient care and enhancing recovery for those who need it most." – Bon-Hi Moon, Professional Practice Leader for Speech-Language Pathology
Trillium Health Partners
THP is committed to delivering high quality and exceptional patient experiences to our community of Mississauga and west Toronto.
Thanks to our Community and Donors
Working with our community and donors, Trillium Health Partners Foundation raises the critical funds needed to address the highest priority needs of Trillium Health Partners.









